‘The NHS shaped my life – now I hope to ensure its future’

The NHS has been a part of my life for as long as I can remember.
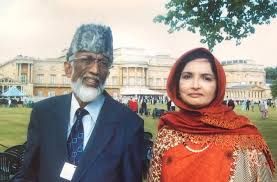
One of my earliest memories is of my late father returning home with a patch over his eye. I was four years old at the time and my father had undergone an operation for glaucoma – the common eye condition that causes damage to the optic nerve. Glaucoma affects over half a million people in the UK, but it tends to show its signs later in life. My Dad wasn’t yet 40 and his eyesight was already deteriorating.
Over the following decade, my father came home with many more eyepatches. NHS doctors tried everything they could to save his sight, but by his late 50s, he was blind.
The NHS, which is celebrating its 75th birthday this week, stayed in our family. After his sight had gone, my father volunteered as a Muslim chaplain in the local hospital. Times were hard but my mother took on a job as an administration assistant in the NHS and worked tirelessly to ensure that we could focus on our studies.
And so, against very long odds, I was able to get into medical school and became an NHS doctor – and I quickly encountered the fundamental struggle that every doctor in our healthcare system experiences. We don’t see our patients until symptoms start showing.
It is too late. Most common diseases start in the body long before they show symptoms. I’ve lost count of the amount of heart attack patients I’ve treated who hadn’t known their arteries had been clogging up for years; or breast cancer patients who were diagnosed at Stage 3, when their chances of surviving for five years or more are 70%, instead of Stage 1, when it’s almost 100%. If only we could have detected them earlier, I could have helped prevent or at least delay these diseases.
Modern healthcare systems – and I don’t just mean the NHS – deal with sickness, not health. That explains why life expectancy in the UK is now around the 80-year mark, but the last 15-20 years of our lives tend to be spent in poor health with 54% of people aged 65 or older living with two or more serious health conditions. By 2035, that figure is expected to rise to 68%.
Glaucoma and a new vision for healthcare
Glaucoma is a good example of what we can do if we see patients before they notice symptoms. Healthcare for the condition has come a long way since my father’s experience in the 1970s. So long as it’s caught early, before the optic nerve gets too damaged, eye specialists can prescribe eyedrops or surgery that stop it in its tracks. Over 90% of people who get treatment for the condition retain useful sight for the rest of their lives.
How do we catch glaucoma early? We regularly test the people who are at risk of the disease. And new advancements in genomics mean we can now identify those people better than ever before. We know where to look in the DNA code to find the signs that someone is likely to develop glaucoma, which means we can offer them the early screening they need.
It doesn’t stop at glaucoma. So many of the common diseases that blight our society can be tackled using the prevention model, from cancer and diabetes to heart disease and stroke. By identifying those at higher risk – through a combination of collecting information about all aspects of their lives and health, as well as their genetics – we can offer earlier screening and treatments to prevent these diseases developing.
That’s why I’m proud to lead Our Future Health. By bringing together up to five million adults from across the country, we’re creating an incredibly detailed picture of the nation’s health. Researchers will use our information to discover new ways to prevent, detect, and treat common diseases.
Each individual volunteer can benefit from it, too as they can opt to receive feedback on their own risk of certain diseases, which could include diabetes, heart disease and glaucoma.
Helping all types of people
Our Future Health can help put the UK at the forefront of preventative healthcare, but to be truly successful we need millions of people to take part. With that level of information, our resource will reflect the UK population, which means people from all ethnic and socio-economic backgrounds will be represented. To help all types of people, we need every kind of person to take part.
And everyone will benefit from it. Preventative healthcare is better for the patient, who stays healthier for longer, and it’s better for the NHS, which would spend less money on costly treatments.
The NHS is an institution that we can be proud of, and its establishment 75 years ago is one of the UK’s greatest achievements. By acting now and working together, we can ensure that our children and grandchildren still benefit from the National Health Service in the 75 years to come.
Dr Raghib Ali is Chief Medical Officer of Our Future Health and an NHS consultant in acute medicine. He was awarded an OBE in the Queen’s Platinum Jubilee Birthday Honours for services to the NHS and Covid-19 response.

Let’s prevent disease together
By volunteering for Our Future Health, you can help health researchers discover new ways to prevent, detect and treat common conditions such as diabetes, cancer, heart disease, stroke and Alzheimer’s.