‘Blood pressure is a silent killer – my appointment with Our Future Health has changed my life’
When Miriam Clark, a 67-year-old retired teacher from south London, joined Our Future Health, she didn’t expect to find herself in A&E less than 24 hours later receiving treatment to lower her blood pressure. “It was like something out of a film,” she said afterwards.
Like millions of other people across the UK, Miriam received an invite to join Our Future Health in the post. She considered joining, but was not a fan of hospitals or needles. After weighing it up for a while, she decided to join to help her grandchildren and the future of medicine.
She saw the day of her appointment at the Croydon clinic as “a little adventure”. “I’m quite a fit person,” she says. “I used to work as a PE teacher.”
As a result, the fact that her blood pressure readings were so high came as a huge shock. “Before I arrived, I was trying to stay calm because I know that every time I have my blood pressure taken, it goes up, plus I have a history of fainting,” says Miriam. “The healthcare assistant was lovely – she kindly took me to lie on a bed before taking my blood and checking my blood pressure and cholesterol.”
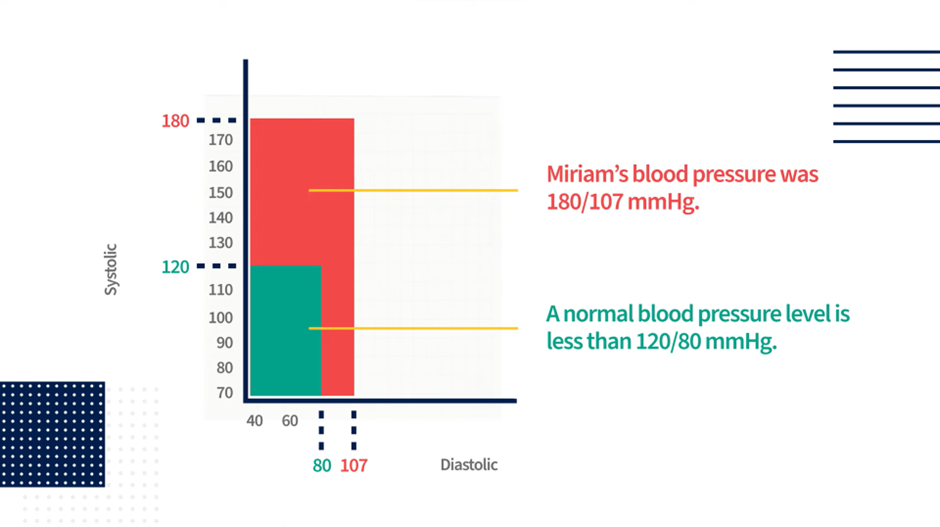
Miriam’s lowest blood pressure reading was 180/107 mmHg. As a guide, the NHS advises that normal blood pressure is usually considered to be between 90/60 mmHg and 120/80 mmHg. “The healthcare assistant said, ‘Oh my goodness.’ Her reaction surprised me – I said, ‘Am I alive?’ She said, ‘Only just!’”
Hospital referral
The healthcare assistant suggested Miriam contact her GP that same day. “I have a blood pressure monitor at home,” says Miriam. “My doctor told me to take three readings in the next 10 minutes. The readings were still high, and it was obviously urgent as the doctor said I needed to go to A&E.
“When I got to A&E, a nurse took my blood pressure and it was even higher.”
By this point, Miriam says that she was feeling terrible – so bad that she had to lie on the A&E floor to stop herself fainting because she was getting worried about how serious her health situation was. “I almost felt like I was at death’s door at this stage,” she remembers.
Doctors gave her medication to bring her blood pressure down and monitored her until it was lower. “Eventually, it came down low enough for them to let me go home,” she says. “Since then, I’ve had to have an echocardiogram and a 24-hour heart monitor to see what my heart’s doing, and I have an appointment to see a cardiologist later in the year.”
The silent killer
High blood pressure, also known as hypertension, is often called the ‘silent killer’ as – like in Miriam’s case – it’s generally symptomless and often picked up late. “People can have high blood pressure for years without realising,” says Dr Raghib Ali OBE, Our Future Health’s Chief Medical Officer. “The first time they find out is when they have a stroke or a heart attack.”
He explains that if you have high blood pressure for a long time, it can accelerate atherosclerosis – where your arteries become narrowed by the build-up of fatty deposits, which can lead to heart attacks and strokes. “It can also cause a blood vessel to burst. If that happens in the brain it’s called a haemorrhagic stroke and it’s extremely serious.”
As a result, high blood pressure is the biggest single contributor to disability and death globally. The World Heart Federation estimates that 1.3 billion people worldwide suffer from hypertension, and it kills 10 million people annually. In the UK, according the British Heart Foundation, four million people under the age of 65 are living with undiagnosed high blood pressure.
Luckily, once detected, high blood pressure can be reversed by making lifestyle changes and/or pharmacological treatments.
Miriam was aware she had heart issues following routine tests five years ago. “A scan showed that the aortic root from the heart was enlarged, so I had to see a cardiologist. I was then informed that I must keep a regular check on my heart and have an echocardiogram every six months. He said it may be nothing, but there’s an operation that can be done if it gets worse.
“I should have gone for the regular examinations, and I didn’t.”
She also has a history of high blood pressure and was put on medication that included beta blockers when she was 60, but she says she reduced the amount she was taking by “self-doctoring”. “I decided that I was OK – I tried to self-diagnose my way out of it. This whole experience has changed the way I behave and think enormously.”
Long-term change

As a result, Miriam is thankful that she joined Our Future Health. “The results have changed my lifestyle – maybe they’ve even saved my life” she said. “It’s reminded me what a silent killer blood pressure can be.”
“I was shocked by my weight because I thought I was a stone lighter than I was, so I aim to lose some pounds. I’ll also have the echocardiograms every six months, and I’m on a higher dosage of medication for my blood pressure.”
As a result of her experience, she’s advising everyone she knows to join Our Future Health. “I had a history of fainting and dislike of hospitals, which put me off having any kind of health checks. But joining Our Future Health has changed my mindset completely. And following these checks, it’s made me feel OK about hospitals, and having my blood taken doesn’t worry me now.
“Signing up is a great thing to do – whether it’s for your children and your children’s children, for yourself, for people in the future that you don’t even know, or for the NHS.”

Let’s prevent disease together
By volunteering for Our Future Health, you can help health researchers discover new ways to prevent, detect and treat common conditions such as diabetes, cancer, heart disease, stroke and Alzheimer’s.